Symptoms of failed implantation can be a frustrating and confusing experience for couples trying to conceive. Implantation is the process of the fertilized egg attaching itself to the uterine lining, and when it fails, it can result in infertility.
Some women may experience symptoms of failed implantation, such as abnormal bleeding, cramping, or spotting.
Understanding the signs of failed implantation is crucial for couples trying to conceive. It can help them identify potential issues and seek medical help if necessary. While some symptoms may be mild and go unnoticed, others may be more severe and require immediate attention.
In this article, we will explore the symptoms of failed implantation, the causes, and the available treatment options.
Key Takeaways
- Failed implantation can result in infertility and cause frustration for couples trying to conceive.
- Symptoms of failed implantation can include abnormal bleeding, cramping, or spotting.
- Understanding the signs and seeking medical help can help couples identify potential issues and explore treatment options.
Understanding Implantation
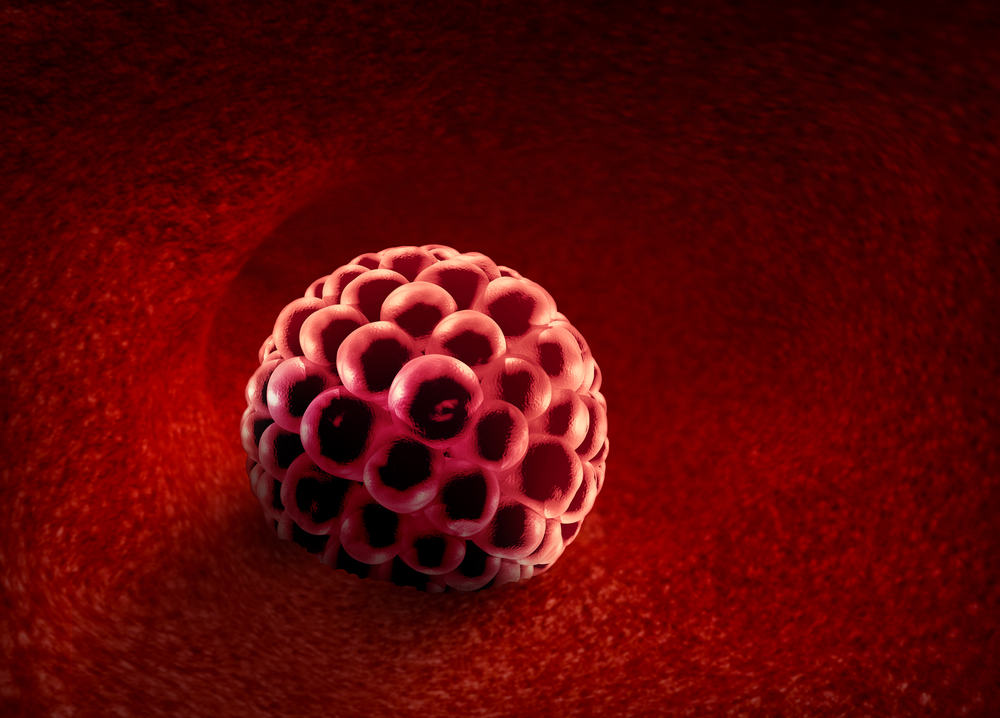
Implantation is a crucial stage in the process of pregnancy. It occurs when the fertilized egg, also known as the blastocyst, attaches itself to the lining of the uterus. The embryo then begins to develop and grow inside the uterus.
Implantation typically occurs around 6 to 10 days after ovulation. During this time, the developing embryo releases pregnancy hormones, such as human chorionic gonadotropin (hCG). These hormones signal to the body that a pregnancy has begun.
The process of implantation is complex and involves many factors. For successful implantation to occur, the embryo must be healthy and the lining of the uterus must be receptive. Factors such as age, health, and lifestyle can all affect the likelihood of successful implantation.
Symptoms of failed implantation can include cramping, spotting, and a delayed or absent period. However, it is important to note that these symptoms can also be caused by other factors and do not necessarily indicate failed implantation.
Overall, understanding implantation is an important part of understanding the process of pregnancy. By knowing what to expect and what factors can affect implantation, individuals can take steps to optimize their chances of a successful pregnancy.
Symptoms of Failed Implantation
Failed implantation refers to a condition where the fertilized egg does not attach itself to the uterine wall. This can occur for a variety of reasons and can result in a failed pregnancy. Some of the symptoms of failed implantation include:
- Bleeding: Light spotting or bleeding can occur during implantation, but if it becomes heavy or prolonged, it can be a sign of failed implantation.
- Cramping: Mild cramping is normal during implantation, but if it is severe or prolonged, it may indicate a problem.
- Lower back pain: This can be a sign of failed implantation, especially if it is accompanied by other symptoms.
- Nausea: While nausea is a common symptom of pregnancy, it can also be a sign of failed implantation.
- Headaches: Headaches can be caused by hormonal changes during pregnancy, but they can also be a sign of failed implantation.
- Constipation: This can be a sign of failed implantation, especially if it is accompanied by other symptoms.
- Premenstrual symptoms: These can include bloating, mood swings, and breast tenderness, and can be a sign of failed implantation.
If you experience any of these symptoms, it is important to speak with your healthcare provider as soon as possible to determine the cause and receive appropriate treatment.
Causes of Failed Implantation
Failed implantation is a common cause of infertility and can be caused by a variety of factors. Some of the most common causes of failed implantation are related to the uterus and the endometrium.
Infections in the uterus can prevent implantation from occurring. Endometriosis can also cause implantation failure due to the growth of tissue outside of the uterus. Additionally, hormonal imbalances can affect the thickness of the uterine lining, resulting in a thin endometrium that is unsuitable for implantation.
Uterine problems such as fibroids and adhesions can also contribute to failed implantation. Fibroid polyps and hydrosalpinges can also cause implantation failure and increase the risk of miscarriage.
Antiphospholipid syndrome is another common cause of failed implantation. This autoimmune disorder can cause blood clots and prevent the embryo from implanting properly.
Overall, there are many potential causes of failed implantation, and it is important to identify and address these issues in order to improve the chances of a successful pregnancy.
Diagnosis of Failed Implantation

When a woman experiences difficulty in conceiving or sustaining a pregnancy, it is essential to diagnose the underlying cause. Failed implantation is one of the most common reasons for infertility, and it is crucial to identify the cause to find the right treatment.
The diagnosis of failed implantation involves a series of tests and evaluations that help identify the cause of the problem. Here are some of the diagnostic tests that may be performed:
1. Pregnancy Test
A pregnancy test is usually the first step in diagnosing failed implantation. A woman can take a home pregnancy test to check if she is pregnant. If the test is positive, it indicates that implantation has occurred.
However, if the test is negative, it could mean that implantation has failed.
2. Hormonal Tests
Hormonal tests are performed to check the levels of hormones such as hCG and progesterone. These hormones play a crucial role in implantation and pregnancy. Low levels of these hormones can indicate a problem with implantation.
3. Ultrasound
An ultrasound is a diagnostic test that uses sound waves to create images of the reproductive organs. It can help identify any abnormalities in the uterus or ovaries that may be causing failed implantation.
4. Hysteroscopy
A hysteroscopy is a minimally invasive procedure that involves inserting a thin, flexible tube with a camera through the cervix to examine the uterus. It can help identify any abnormalities, such as fibroids or polyps, that may be preventing implantation.
5. Endometrial Biopsy
An endometrial biopsy involves removing a small sample of the lining of the uterus for examination. It can help identify any abnormalities in the lining that may be preventing implantation.
6. Gestational Sac
A gestational sac is a fluid-filled structure that develops in the uterus after implantation. An ultrasound can detect the presence of a gestational sac, which indicates that implantation has occurred.
In conclusion, diagnosing failed implantation involves a series of tests and evaluations that help identify the underlying cause. It is essential to work with a healthcare provider to determine the appropriate diagnostic tests and find the right treatment.
In Vitro Fertilization and Implantation
In vitro fertilization (IVF) is a fertility treatment that involves fertilizing an egg with sperm outside of the body, in a laboratory setting. This procedure is typically used when other methods of fertility treatment have failed. IVF is often used in combination with other treatments, such as egg donation.
During the IVF process, eggs are retrieved from the woman’s ovaries and fertilized with sperm in a laboratory dish. The resulting embryos are then transferred to the woman’s uterus, where they may implant and grow into a pregnancy.
One of the main advantages of IVF is that it allows doctors to carefully control the fertilization and implantation process. This can help to increase the chances of a successful pregnancy, particularly for couples who have struggled with infertility for a long time.
However, IVF is not always successful. In some cases, the embryos may fail to implant in the uterus, which can result in a failed pregnancy. Some common symptoms of failed implantation include:
- Heavy bleeding or spotting
- Cramping or abdominal pain
- Changes in vaginal discharge
- A sudden decrease in pregnancy symptoms
If you are experiencing any of these symptoms, it is important to speak with your doctor as soon as possible. They may be able to provide you with additional information and support, as well as recommend additional treatments or procedures that may increase your chances of a successful pregnancy.
Overall, IVF can be an effective treatment option for couples struggling with infertility. However, it is important to carefully consider all of your options and to work closely with your doctor to develop a treatment plan that is right for you.
Treatment and Prevention of Failed Implantation

When it comes to treating and preventing failed implantation, there are several options available.
Firstly, it is important to address any underlying medical conditions that may be contributing to the problem. This can include surgery to correct any structural issues in the reproductive system, or medication to regulate hormonal imbalances.
Lifestyle factors can also play a role in failed implantation. Smoking, for example, can decrease fertility and increase the risk of miscarriage, so quitting smoking is strongly recommended.
Maintaining a healthy weight through a nutritious diet and regular exercise can also improve fertility.
For those undergoing fertility treatments, working with a fertility specialist can help identify any potential issues and develop a treatment plan. This may include using assisted reproductive technologies such as in vitro fertilization (IVF) or surrogacy.
In addition to medical interventions, there are also natural methods that can be used to improve the chances of successful implantation. Tracking basal body temperature and monitoring hormone levels can help pinpoint the optimal time for conception.
Making lifestyle changes such as reducing stress and getting enough sleep can also improve fertility.
Overall, the key to preventing failed implantation is to address any underlying medical conditions and make lifestyle changes that support healthy fertility. By working with a healthcare provider and making informed choices, individuals can increase their chances of a successful pregnancy.
Emotional Impact of Failed Implantation
Failed implantation can be emotionally devastating for couples trying to conceive. It is common for women to feel a sense of loss, disappointment, and sadness. The emotional impact of failed implantation is often compared to that of early pregnancy loss or chemical pregnancy.
It is important for couples to understand that failed implantation is not their fault. It is a natural part of the conception process and can happen to anyone. It is also important for couples to communicate their feelings with each other and seek support from family, friends, or a therapist.
Some common emotions that women may experience after failed implantation include:
- Sadness
- Disappointment
- Guilt
- Anger
- Frustration
- Anxiety
It is important for women to take care of themselves emotionally during this time. This may involve taking time off work, engaging in self-care activities, and seeking professional help if necessary.
In conclusion, failed implantation can have a significant emotional impact on couples trying to conceive. It is important for couples to understand that it is a natural part of the conception process and to seek support from each other and from professionals if necessary.
Failed Dental Implantation
Dental implants are a popular and effective way to replace missing teeth. However, in some cases, the implant may fail to integrate with the surrounding bone, leading to failed implantation.
One potential cause of failed implantation is poor oral hygiene. If the implant site is not kept clean, bacteria can build up and cause infection, which can prevent proper osseointegration. Additionally, gum disease can weaken the bone and prevent successful implantation.
Another possible cause of failed implantation is osteoporosis, a condition that weakens the bones. Patients with osteoporosis may not have enough bone density to support the implant, leading to implant failure. In these cases, a bone graft may be necessary to strengthen the bone before the implant can be placed.
Swelling and pain around the implant site can also be signs of failed implantation. X-rays may be necessary to determine if the implant has properly integrated with the bone. If the implant has failed, it may need to be removed and replaced.
In some cases, the abutment or crown may be the cause of implant failure. If the abutment is not properly fitted or if the crown is too large or too small, it can prevent proper osseointegration and lead to implant failure.
Overall, proper oral hygiene and regular dental check-ups can help prevent failed implantation. Patients should also be aware of the potential risks and complications associated with dental implants and discuss any concerns with their dentist.
Role of Vitamins and Minerals in Implantation
A successful pregnancy relies on a complex interplay of factors, including the health of the egg and sperm, the function of the uterus, and the ability of the embryo to implant and develop properly.
Vitamins and minerals play a crucial role in supporting these processes, and deficiencies in these nutrients can increase the risk of failed implantation.
One key nutrient for implantation is vitamin D. This vitamin is involved in a range of physiological processes, including bone health, immune function, and cell growth and differentiation.
Recent research suggests that low levels of vitamin D may be associated with reduced fertility and increased risk of miscarriage. In addition, vitamin D may play a role in regulating the menstrual cycle and promoting uterine receptivity, both of which are important for successful implantation.
Other important nutrients for implantation include folic acid, iron, and zinc. Folic acid is essential for proper neural tube development in the fetus, and deficiencies in this nutrient can increase the risk of birth defects.
Iron is necessary for the production of hemoglobin, which carries oxygen to the developing fetus, while zinc is involved in DNA synthesis and cell division.
It is important to note that while vitamin and mineral supplements can be helpful in supporting implantation and pregnancy, they should not be used as a substitute for a healthy diet. Women who are trying to conceive should aim to consume a balanced diet rich in fruits, vegetables, whole grains, and lean protein sources.
In addition, they should speak with their healthcare provider about any concerns they may have regarding nutrient deficiencies or supplementation.
Related Posts:
Frequently Asked Questions
What are the signs of unsuccessful implantation?
There are several signs of unsuccessful implantation, including light bleeding or spotting, cramping, and a negative pregnancy test. However, it is important to note that these symptoms may also occur in a normal menstrual cycle.
How long after implantation failure will my period start?
If implantation fails, it usually takes about two weeks for the body to recognize that the embryo has not implanted and for the menstrual cycle to begin. However, this timing can vary from woman to woman.
Can failed implantation cause an early period?
Yes, failed implantation can cause an early period. This is because the body recognizes that the embryo has not implanted and begins the menstrual cycle.
What happens if an embryo fails to implant?
If an embryo fails to implant, it will be naturally expelled from the body during the menstrual cycle. This is a normal process and does not usually require medical intervention.
How to prevent implantation failure?
There are several steps that can be taken to prevent implantation failure, including maintaining a healthy weight, avoiding smoking and excessive alcohol consumption, and managing stress levels. It is also important to follow any instructions provided by a fertility specialist.
What are the next steps after a failed implantation?
After a failed implantation, it is important to discuss next steps with a fertility specialist. Depending on the individual situation, options may include trying again with a different embryo, exploring alternative fertility treatments, or considering adoption or other options for building a family.

Iesha is a loving mother of 2 beautiful children. She’s an active parent who enjoys indoor and outdoor adventures with her family. Her mission is to share practical and realistic parenting advice to help the parenting community becoming stronger.